 VOLUME 26, ISSUE 4 • DECEMBER 2022 Full issue »
VOLUME 26, ISSUE 4 • DECEMBER 2022 Full issue »

GOLD Award for the Best Review Article in Movement Disorders Clinical Practice:
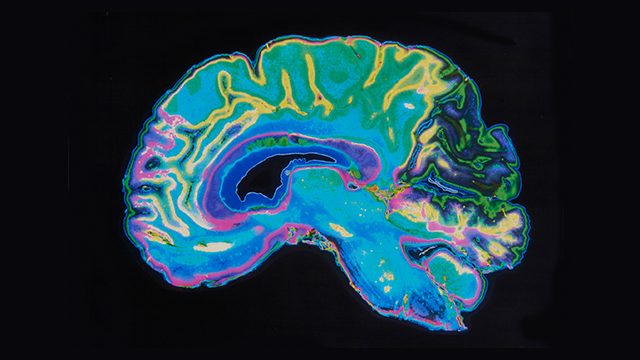
Pragmatic Approach on Neuroimaging Techniques for the Differential Diagnosis of Parkinsonisms
Being recognized as the most impactful research and review article published in Movement Disorders Clinical Practice in the 2021-2022 term is one of the highest honors that study group members can aspire to as part of their work dedicated to the neuroimaging field in parkinsonisms.
From the days we started as members of the MDS Neuroimaging Study Group and in our annual meetings, we had discussions about how the neuroimaging field evolved to change the role of imaging from merely excluding secondary causes of parkinsonisms to aiding in the differential diagnosis. We also realized that the increasing recognition of imaging techniques contrasted with the lack of imaging protocols or algorithms about how to use them in daily practice for differential diagnosis.
This is particularly relevant in the scenario of the recently reviewed diagnostic criteria for Parkinson´s disease (PD) and atypical parkinsonisms (APDs), which are moving slowly to incorporate imaging as part of their criteria. The MDS diagnostic criteria for PD include the novelty of incorporating imaging as part of “absolute exclusion criteria” (normal presynaptic dopaminergic terminal scan) and “supportive criteria” (cardiac sympathetic denervation using (123)I metaiodobenzyl guanidine) and the use of cerebral glucose metabolism with [18F]FDG-PET that has been supported by the MDS criteria for the diagnosis of progressive supranuclear palsy (PSP) and the latest criteria for the diagnosis of multiple system atrophy (MSA).

It so happened that we decided to write this paper to build a consensus on how to use imaging techniques in daily practice by delineating a pragmatic approach to describe the basic steps that may not be missed in clinical practice for the diagnosis and differential diagnosis of parkinsonisms. This led us to assemble the imaging findings that support the diagnosis of PD or APDs with clinical aspects through 2 algorithms, one for MRI and another for PET/SPECT imaging, with a strong focus in visual examples that fit with vignettes depicting the imaging findings that support their diagnosis.
Nowadays, high-field MR using qualitative techniques of neuromelanin and dorsal nigral hyperintensity imaging allow the identification of the ongoing neurodegenerative process, and the molecular imaging field gives us the possibility of imaging protein aggregation. In this regard, DAT-SPECT was approved by the FDA for the differential diagnosis of PD from essential tremor, although other markers of presynaptical dopaminergic function are used in clinical practice. [18F]FDG-PET studies are especially relevant because they provide “patterns of brain hypometabolism,” offer a strong “imaging–clinical” correlation to the clinician, and are widely available in clinical practice.
Tau PET imaging is the most challenging area in parkinsonisms that may evolve as an in vivo modality supportive of the pathological PSP diagnosis at the individual level, as shown by second-generation tracers such as [18F]-PI-2620, which demonstrated high in vitro binding affinity for aggregated 4-repeat isoforms and no substantial off-target binding to β-amyloid or MAO-A or B, highlighting that patients with PSP presented significant elevation of tracer binding in PSP target regions.
We would very much hope that this pragmatic imaging-based diagnostic approach based on current experience and published literature becomes established in Neurologic and Movement Disorder clinics to guide the use of imaging methods to contribute to a modern concept of neurodegenerative diseases, where biomarkers are integrated with clinical criteria.
If you want to hear more about this paper, MDS podcast also interviewed the author.
Read more Moving Along:






