Value of Neuropathology in Atypical Parkinsonism
Date: January 2023
Prepared by SIC Member: Ece Bayram, MD, PhD
Authors: David Coughlin MD, MTR; Melissa Murray, PhD.; Shunsuke Koga, MD, PhD; and Gabor G. Kovacs MD PhD.
Editor: Lorraine Kalia, MD, PhD.
Introduction
Atypical parkinsonisms are movement disorders that can resemble Parkinson’s disease, although they often progress faster and are associated with several motor and non-motor symptoms uncharacteristic of Parkinson’s disease. This group of neurodegenerative diseases include multiple system atrophy (MSA), progressive supranuclear palsy (PSP), corticobasal degeneration (CBD) and dementia with Lewy bodies, all of which require specific pathological findings to make a definitive diagnosis. Although the traditional clinicopathological diagnosis still maintains its importance in parkinsonian disorders, advances in the field of neuropathology have been shaping our understanding of the pathophysiology in atypical parkinsonisms as well as guiding our search for biomarkers and treatment targets. Here, Drs. David Coughlin, Melissa Murray, Shunsuke Koga and Gabor Kovacs discuss the role of neuropathology in atypical parkinsonisms beyond diagnosis and anticipated advances in research as well as outline the current status of brain donations globally.
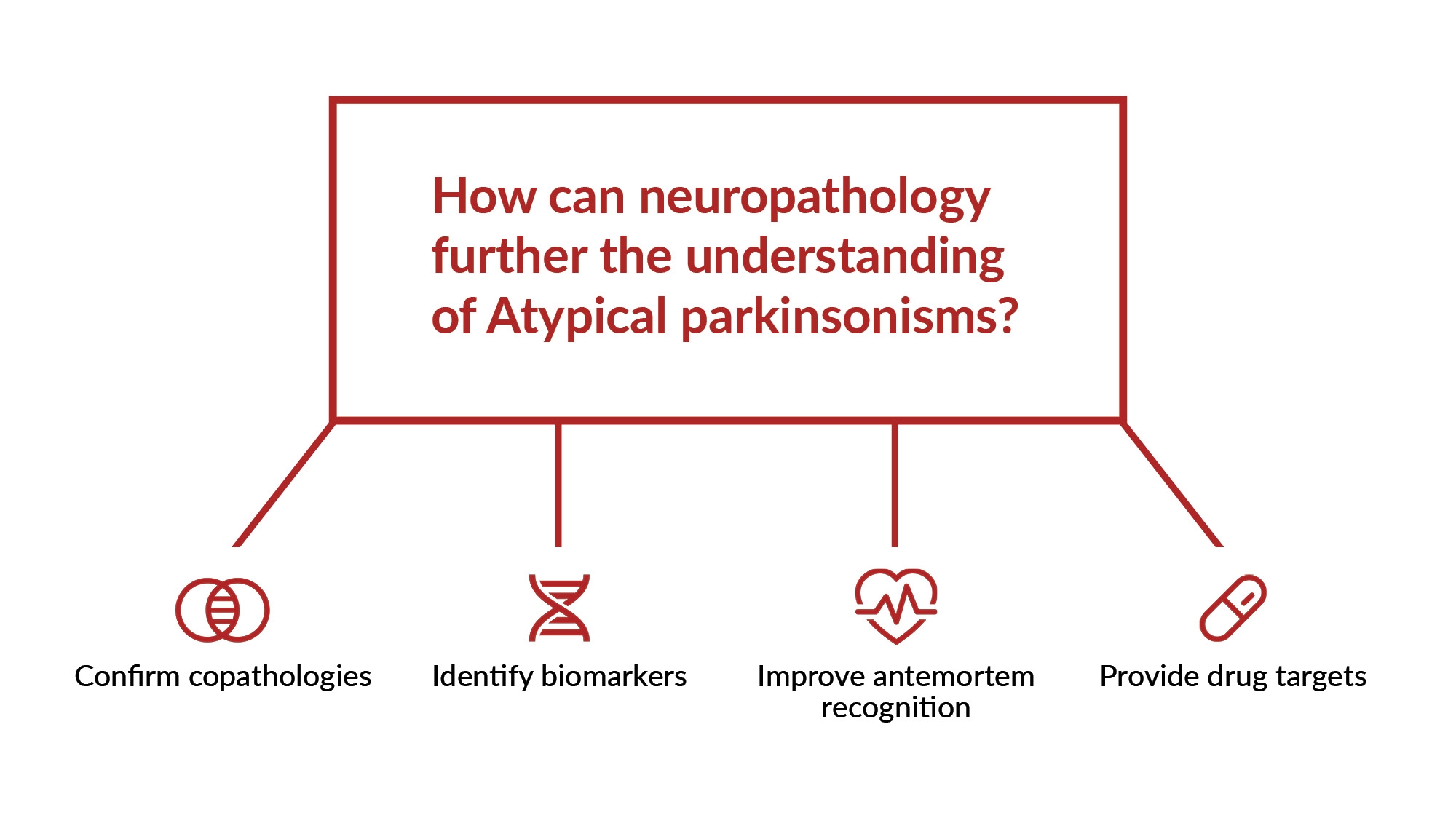
1. Beyond traditional pathological diagnosis, what additional information can neuropathology provide for atypical parkinsonisms?
Dr. Kovacs:
Neuropathology is able to help discover new morphological phenotypes that help us understand the variability in clinical courses. Together with complementary methods such as biochemistry and cryo-EM and seeding assays this helps us to understand more precisely neurodegenerative proteinopathies. There are still ‘unexpected’ results in neuropathology, which means that the clinical suspicion and the neuropathology results might be different. This is particularly true for clinically ‘atypical’ phenotypes and parkinsonism. We still have to understand the spectrum of combined/mixed pathologies and their clinicopathological relevance. Without neuropathology, this cannot be achieved yet. Recent developments in biomarkers, neuroimaging (including PET ligands) and even therapy trials need feedback from neuropathology for quality reasons and eventually to describe the effects/side effects of therapies. The classical clinicopathological discussions are still a very effective way of quality control for clinicians and education of the new generation of neurologists
Dr. Koga:
Most importantly, neuropathology is the only way to confirm the diagnosis of atypical parkinsonian disorders. The clinical diagnosis of atypical parkinsonisms is challenging, and neuropathologic and clinical diagnoses sometimes differ. For example, it is not uncommon for a patient thought to have PSP clinically to be found to have MSA pathology at autopsy. It is crucial to confirm the diagnosis and provide the results to clinicians and patients’ families. Neuropathology can not only confirm the diagnosis but also evaluate the concomitant pathology. For example, many patients with PSP have not only tau pathology but also a variety of other pathologies, including cerebrovascular disease, Alzheimer's disease neuropathologic changes (e.g., neurofibrillary tangle and amyloid plaques), and TDP-43 pathology. One of the future challenges is evaluating the impact of these comorbid pathologies on clinical presentations and the extent and distribution of tau pathology.
Dr. Murray:
Neuropathology provides the ground truth when evaluating neurodegenerative diseases. As biomarkers continue to improve antemortem recognition of abnormal changes, neuropathology remains critical to confirm clinical suspicions and evaluate microscopic distribution of pathology that may have impacted clinical presentations. As Dr. Koga suggested, neuropathologic lesions are strategic and may masquerade as a clinical syndrome inconsistent with expected neuropathology. Moreover, neuropathologic evaluation of lesions in atypical parkinsonisms provides insight into the spatial biology of neuronal and glial interactions, laminar distributions, and environment surrounding neurosurgical interventions (e.g., deep brain stimulation).
Dr. Coughlin:
The most recent clinical criteria for MSA, CBD, and PSP have fairly high positive predictive values when compared to pathological diagnoses. But errors still occur in clinical diagnoses, even in patients who have been followed for many years. In vivo biomarkers that can aid in differentiating atypical parkinsonisms with similar phenotypes are still being researched and many are not readily available in most clinics (i.e., second generation tau PET, cardiac MIBG scintigraphy, alpha-synuclein skin immunofluorescence, CSF seeding amplification assays, etc). So, even now, pathological examination remains gold-standard for the diagnosis of atypical parkinsonisms; furthermore, the study of patients with autopsy-validated diagnoses provide extremely valuable information about their clinical course and biomarker profiles during life.
Beyond the categorical information gleaned from a pathological diagnosis, pathological examinations can provide information about the brain regions affected by disease. This allows for better understanding of vulnerable networks and regions that show these changes which can suggest mechanisms of pathological spread. There is a published staging system for PSP neuropathology but there are less well-defined staging systems for MSA and CBD and typically reports will just describe the regions affected by proteinaceous aggregates. Further study is needed to define staging systems for other atypical parkinsonisms.
Pathological examination also can reveal the presence of other co-pathologies like cerebrovascular disease, Alzheimer’s disease neuropathological changes, and TDP-43 inclusions. While it is well documented in a large body of literature that most autopsied brains will contain more than one neuropathology, this knowledge is not often applied in clinical assessments or biomarker characterization of patients. How co-pathologies may or may not influence the clinical course of atypical parkinsonisms or how co-pathologies may mechanistically interact with a primary atypical parkinsonian pathology is not fully understood.
Lastly, the above comments are relegated to assessments using traditional immunohistochemical staining techniques on fixed tissue for well-known entities like tau, alpha-synuclein, amyloid-beta, and TDP-43. There is a myriad of information that can be gleaned from assessment of other proteins and isoforms as well (i.e., 4R tau and 3R tau isoforms, microglia, markers of inflammation, assays for oligomeric proteins and many more). Yet even more information can be gained from frozen tissue where other techniques like RNA-seq and tau or alpha-synuclein seeding amplification assays can be applied.
2. What do you foresee as the upcoming advances in neuropathology of atypical parkinsonisms?
Dr. Murray:
In this exciting biomarker era, we are looking forward to 3R tau, 4R tau, and alpha-synuclein specific PET radioligands and fluid measures. Through neuropathologic validation of emerging neuroimaging biomarkers, it will be fascinating to better appreciate the spatial distribution in autopsy confirmed series. Regarding temporality of atypical parkinsonian disorders, it will be especially interesting to observe the sensitivity of fluid biomarkers early in the clinical course compared to timing of neuroimaging-derived biomarker changes. On a microscopic level through the advent of spatial biology techniques, including spatial proteomics and spatial transcriptomics, the field should expect to see a deeper understanding of neuronal and glial interactions. Uncovering underlying protein and gene expression changes in the context of disease severity will hopefully provide mechanistic insight into cause and effect which more traditional bulk sequencing methods may not capture.
Uncovering underlying protein and gene expression changes in the context of disease severity will hopefully provide mechanistic insight into cause and effect which more traditional bulk sequencing methods may not capture.”
—Melissa E. Murray, PhD
Dr. Coughlin:
I think that continued work on the ultrastructural composition of tau and alpha-synuclein in atypical parkinsonisms through electron microscopy is interesting and adds to our knowledge beyond the regions, cell-types, and morphology of protein aggregates. Seeding amplification assays like real-time quaking induced conversion (RT-QuIC) and protein misfolding cyclic amplification (PMCA) are assays that make use of the templating capacity of pathological alpha-synuclein and tau ‘seeds’. These assays are under development as in vivo biomarkers in CSF and peripheral tissue but using these assays to measure seeding activity directly from brain tissue is providing interesting information about tau and alpha-synuclein seeding activity in atypical parkinsonisms. How atypical parkinsonisms may be affected by TMEM106B, a protein involved in lysosomal function with aggregates being seen across multiple neurodegenerative diseases, is also a developing story. Lastly, studying the relationship between neuropathology and biofluid biomarkers and new PET ligands will be of great importance.
The use of digital image analysis techniques can offer additional information to the ratings and descriptions that you get from traditional pathologic assessments. Broadly speaking, in this approach, immunohistochemically stained slides undergo high resolution scanning to produce a large image file. Software programs can then be used to detect how much pathological signal there is in a region. This provides finely-grained and somewhat more objective measurements that can be useful for biomarker-pathological correlative studies. There are several groups who are working on methods to quantify pathological burden or use feature detection to identify certain types of inclusions. It is currently not clear how some of these techniques may scale for multi-centered studies but, in instances where similar staining and digital histological methods are used, there appears to be similar patterns of pathology across institutions.
Dr. Koga:
Several areas of research and potential advances in neuropathology may be relevant to the diagnosis and understanding of atypical parkinsonisms. Developing more sensitive and specific biomarkers for the diagnosis of atypical parkinsonisms, such as protein aggregates or other markers of neurodegeneration or neuroinflammation. As with Alzheimer's disease, for which several reliable biomarkers, neuroimaging or fluid biomarkers are under development for atypical parkinsonism. For example, positron emission tomography (PET) that can visualize tau in vivo can non-invasively assess the distribution and severity of tau pathology and monitor disease progression in atypical parkinsonisms. To achieve this, neuropathology can provide validation studies on whether these biomarkers correctly diagnose the underlying pathology of these atypical parkinsonisms.
Dr. Kovacs:
My list would be (1) Neuropathology with immunostainings for a wide range of protein modifications: this is important also to develop in vivo assays and to provide feedback for existing in vivo diagnostic assays; (2) 3D reconstruction of protein deposits in the brain; (3) molecular imaging to map protein localizations in a super-resolution; (4) development of AI methods to quantify protein deposition in a more objective and precise way; (5) methods evaluating seeding behavior or proteins associated with atypical parkinsonism: this is important also to develop in vivo assays; and (6) ultrastructural studies, including cryo-Electron microscopy to understand the basis of variability on an atomic level: this is important if we want to target proteins for therapy.
3. What is the state of brain donations across the globe? What are the major challenges and their potential solutions? (For example, are there challenges with lack of support, lack of access or diversity, lack of data in different geographical locations?)
Dr. Coughlin:
Brain donation programs are largely restricted to large academic centers and many require enrollment in other research studies to be able to participate in brain donation. There is an awful lot of infrastructure that goes into creating and maintaining a brain donation program and brain bank. Institutional and grant support are essential. There are often significant issues with lack of diversity in brain banks as brain donation participants tend to be those who are accessing care at tertiary care academic hospitals and who are participating in these research studies. There are some initiatives that are seeking to begin to remedy some of this by focusing on recruiting underrepresented populations to brain donation programs and the knowledge gained from a more diverse set of subjects will be extremely helpful to understand the spectrum of disease in atypical parkinsonisms and to determine if there are meaningful differences across different racial and ethic groups. There are some national organizations in the United States like the NIH biobank and CurePSP’s brain donation program where patients can donate their brains if there is not a local brain bank. In general though, the more information that is available from a patient, be it clinical history, blood samples, spinal fluid, or imaging data to pair with a brain donation, the better. Furthermore, there is some variability in which brain regions are sampled and which stains are applied between brain banks and some degree of harmonization in these methods would be useful to aid in multi-centered studies.
Dr. Kovacs:
Established brain donation systems can be found on all continents with some predominance in North America and Europe. The major challenge is organizing long-term funding and finding neuropathologists who evaluate the cases in the brain banks on a high quality. To overcome this challenge, clinicians and scientists have to stand up to find support for brain banks: without clinicians’ commitment and support actually it is impossible to run a brain donation program. Science politics has to understand the relevance of brain donations so better public relations is needed to inform them. Regular quality control of neuropathology evaluations of brain banks should be organized. There is a need for multicentric case-evaluations, quality control of stainings, harmonization of and standardization of methods used in various brain banks around the globe and regular education of neuropathologists working for brain banks.
The major challenge is organizing long-term funding and finding neuropathologists who evaluate the cases in the brain banks on a high quality.
—Gabor G. Kovacs MD PhD
Dr. Koga:
There is significant variability in the availability of brain donations for research and diagnosis across the globe. In some countries, there are well-established brain banks and a strong tradition of brain donation, while there are only a few brain banks in low- and middle-income countries. The lack of brain banks in developing countries can be attributed to various reasons. Since brain banking and neuropathologic assessment requires a high degree of expertise, a lack of qualified personnel may be one of the most common reasons. Brain banks in these countries may also face challenges due to limited funding and access to resources and technology, which can hinder their ability to process and store brain tissue effectively and restrict the research scope. Cultural and social factors cannot be ignored. Attitudes toward brain donation can vary widely, and there may be cultural or religious beliefs that discourage or prohibit brain donation. The level of education also influences the willingness to consent to an autopsy. Many people may not be aware of the importance of brain donation or how to go about it. Potential solutions to these challenges include (1) educating the public about the importance of brain donation and how it can contribute to medical research and advances; (2) engaging with community organizations, religious leaders, and other influencers to promote brain donation and address any concerns or misconceptions; and (3) working with policymakers to develop transparent and fair guidelines and sufficient budget for brain donation that consider the needs of donors, their families, and the scientific community.
Dr. Murray:
Brain donation is the ultimate gift. From my personal experience with donating my grandmother’s brain, our family found closure and the sense that the legacy of her disease would contribute toward prevention and/or finding a cure. My grandmother, or rather the data derived from her brain tissue, has traveled the world with me as a part of many of my studies. As I am a huge advocate for brain donation, I am very interested to learn from others about their hesitancies or hesitancies they translate on behalf their families and communities. Dr. Koga excellently captured the complexity of challenges across the globe. Brain banks require an immense of amount of funding, dedicated personnel, and longevity of an institution. As such, many center around longitudinal studies that enable the longitudinal data and biomarker collection that compliments neuropathologic phenotyping. Increasing awareness through social media, popular culture, and by simply having conversations could make for a much brighter future that enables global participation.
Further readings
-
Coughlin DG, Goodwill VS, Standke HG, Kim Y, Coley N, Pizzo DP, et al. Selective tau seeding assays and isoform-specific antibodies define neuroanatomic distribution of progressive supranuclear palsy pathology arising in Alzheimer’s disease. Acta Neuropathol. 2022 Oct;144(4):789–92.
-
Spotorno N, Coughlin DG, Olm CA, Wolk D, Vaishnavi SN, Shaw LM, et al. Tau pathology associates with in vivo cortical thinning in Lewy body disorders. Ann Clin Transl Neurol. 2020;
-
Coughlin DG, Ittyerah R, Peterson C, Phillips JS, Miller S, Rascovsky K, et al. Hippocampal subfield pathologic burden in Lewy body diseases vs . Alzheimer’s disease. Neuropathol Appl Neurobiol. 2020 Dec 24;46(7):707–21.
-
Coughlin DG, Xie SX, Liang M, Williams A, Peterson C, Weintraub D, et al. Cognitive and Pathological Influences of Tau Pathology in Lewy Body Disorders. Ann Neurol. 2019 Feb;85(2):259–71.
-
Koga S, Aoki N, Uitti RJ, et al. When DLB, PD, and PSP masquerade as MSA: an autopsy study of 134 patients. Neurology 2015;85:404-412.
-
Jecmenica Lukic M, Kurz C, Respondek G, et al. Copathology in Progressive Supranuclear Palsy: Does It Matter? Mov Disord 2020;35:984-993.
-
Koga S, Ghayal NB, Dickson DW. Deep Learning-Based Image Classification in Differentiating Tufted Astrocytes, Astrocytic Plaques, and Neuritic Plaques. J Neuropathol Exp Neurol. 2021 Mar;80(4):306–12.
-
Ferman TJ, Aoki N, Crook JE, Murray ME, Graff-Radford NR, van Gerpen JA, et al. The limbic and neocortical contribution of α-synuclein, tau, and amyloid β to disease duration in dementia with Lewy bodies. Alzheimer’s Dement. 2018;14(3):330–9.
-
Coughlin DG, Hiniker A, Peterson C, Kim Y, Arezoumandan S, Giannini L, et al. Digital Histological Study of Neocortical Grey and White Matter Tau Burden Across Tauopathies. J Neuropathol Exp Neurol. 2022 Nov;81(12):953–64.
-
Krishnamurthy S, Mathews K, McClure S, Murray M, Gilcrease M, Albarracin C, et al. Multi-Institutional Comparison of Whole Slide Digital Imaging and Optical Microscopy for Interpretation of Hematoxylin-Eosin–Stained Breast Tissue Sections. Arch Pathol Lab Med. 2013 Dec;137(12):1733–9.
-
Dugger BN, White III C, Stahly B, Schneider JA, Robichaud E, Reichard RR, et al. The status of digital pathology and machine learning within Alzheimer’s Disease Centers. Alzheimer’s Dement. 2020 Dec;16(S2):e043916.
-
Akinyemi RO, Salami A, Akinyemi J, et al. Brain banking in low and middle-income countries: Raison D'etre for the Ibadan Brain Ageing, Dementia And Neurodegeneration (IBADAN) Brain Bank Project. Brain Res Bull 2019;145:136-141.
-
Oluwasola OA, Fawole OI, Otegbayo AJ, Ogun GO, Adebamowo CA, Bamigboye AE. The autopsy: knowledge, attitude, and perceptions of doctors and relatives of the deceased. Arch Pathol Lab Med 2009;133:78-82.







