 VOLUME 29, ISSUE 4 • DECEMBER 2025.
VOLUME 29, ISSUE 4 • DECEMBER 2025.

Cell-type specific bidirectional modulation of STN neurons rescue parkinsonian motor symptom
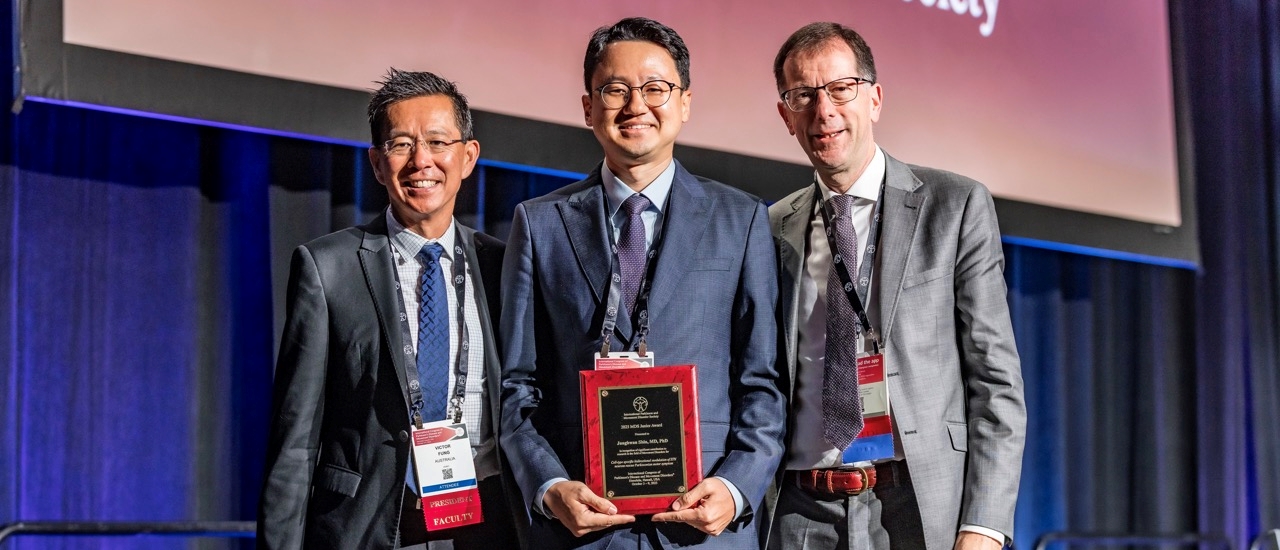
Winning the Junior Award at the 2025 MDS Congress was truly one of the dream-come-true moments of my career. Since my first participation in MDS in Stockholm in 2014, I have witnessed many outstanding young researchers receive this honor, and over the years, I’ve also watched the awardees grow into leading researchers who shape the field beyond the cutting edge. To actually receive the award felt surreal; I could not at first believe the notification, and I remember asking if there was any mistake and if it was true. The best part of receiving the award was bringing my wife and son to the award lectures, and I had a chance to introduce my work to my family.
I remember the day I chose neurology as my future career. During my internship in the Department of Anesthesiology, I witnessed my first DBS surgery in June 2010. I still vividly remember that moment: The patients were awakened during the procedure, and I saw the dramatic effect of DBS on the tremor of patients with Parkinson’s disease. The patient was in tears, and I did not expect such a profound moment as I was sitting behind the anesthesia machine. That single experience made me want to understand movement disorders more deeply and motivated me to seek mentors who could guide me. Meeting Professor Beomseok Jeon (BJ) was pivotal; his mentorship shaped my path and introduced me to the world of clinical neurology and movement disorders. As a neurology resident, I had the opportunity to see many PD patients with DBS, and I began to observe the remarkable benefits of stimulation, both in the short and long term. At first, I even wondered why we needed to study the mechanisms of DBS when it already worked so well clinically. But over time, I realized how little we actually understood about the underlying neurophysiology.
This unmet need led me to pursue a full-time PhD at the Korea Advanced Institute of Science and Technology (KAIST), where I immersed myself in basic neuroscience of the basal ganglia using novel technologies such as single-unit electrophysiology, optogenetics, and in-vivo calcium imaging. My work focused on understanding the mechanisms of the basal ganglia through functional dissection of its circuits.
When I returned to the hospital after completing my PhD, I became more deeply involved in treating patients with Parkinson’s disease using deep brain stimulation (DBS) as a clinical fellow under Professor BJ. With more experience, I began to see things I hadn’t appreciated before. In addition to witnessing significant clinical improvements, I also encountered the non-motor side effects that some patients experience. The more I saw patients struggle with cognitive or mood-related side effects after bilateral STN DBS, the more my curiosity grew — eventually becoming a conviction: To improve outcomes, reduce side effects, and design the next generation of neuromodulation therapies, we must first understand the precise circuits we are modulating. It was during this period that the idea for my award-winning project began to take shape. Emerging evidence suggested that the subthalamic nucleus (STN) was far more heterogeneous than traditionally believed. Thanks to the discovery of my co-worker Jinny Kim from KIST, we could understand the cellular subtypes within STN. We hypothesized specific cell types (parvalbumin-expressing neurons) could be more involved in motor symptoms in Parkinson disease based on topographical distribution and electrophysiological properties.
Over nearly three years of work, using multiple Parkinsonian mouse models and advanced circuit-modulation tools, my team and I uncovered compelling evidence that selectively modulating parvalbumin neurons could rescue parkinsonian motor symptoms, while modulating other subpopulations within the STN did not produce benefits in motor deficits in the PD model. These findings strengthened the idea that future neuromodulation may be far more precise, targeting specific cellular subtypes to enhance benefit while minimizing side effects. If validated across models and expanded with newer technologies, such insights could eventually guide next-generation DBS systems capable of stimulating only the most therapeutic microcircuits while sparing those that contribute to cognitive or emotional adverse effects. This could fundamentally reshape how we personalize DBS programming in the future.
Receiving the Junior Award is not just a personal milestone, but also a reminder of why scientific curiosity and perseverance are so important. I hope my journey encourages other young researchers to follow their questions with passion. Sometimes, a single moment of inspiration — such as my first DBS surgery — can transform a career. And sometimes, dreams really do come true. I would like to thank all my colleagues and lab members, especially Professor BJ for his guidance throughout my career. And finally, I would like to express my sincere appreciation to my family for their unwavering support.
You can view the 2025 plenary session recordings, including the Junior Award lectures, through April 30, 2025.
Listen to a podcast interview about this abstract: ![]() Listen now
Listen now
Read more Moving Along:






