 VOLUME 27, ISSUE 2 • JUNE 2023 Full issue »
VOLUME 27, ISSUE 2 • JUNE 2023 Full issue »

The accuracy of the clinical diagnosis of multiple system atrophy (MSA) has been suboptimal due to overlapping symptoms with other neurodegenerative disorders, especially in the early stages of the disease, with misdiagnosis rates ranging from 21-38% 2-4. The International Parkinson and Movement Disorder Society (MDS) recently published new clinical diagnostic criteria for MSA, which aim to improve diagnostic accuracy in clinical practice and research 5.
These criteria include four levels of diagnostic certainty: |
|
Compared to the previous second consensus criteria, it has been updated with the inclusion of neuropathological evidence to replace the definite MSA category. Clinically established MSA requires autonomic dysfunction and poorly L-dopa-responsive parkinsonism or cerebellar syndrome and must include MRI markers. Clinically probable MSA requires at least two core features of autonomic dysfunction, parkinsonism, and cerebellar impairment. Both categories require supportive motor or nonmotor features and the absence of exclusion criteria.
In this clinicopathological study, we evaluated the accuracy and diagnostic properties of these new criteria in a large cohort of pathology-proven patients with MSA and a control group of patients with parkinsonism and / or cerebellar ataxia. We retrospectively reviewed the medical records and applied the MDS diagnostic criteria for MSA, previous consensus criteria and recorded diagnosis in clinical practice at the early (within 3 years of motor symptom onset) and final stages of the disease.
Our results showed an overall excellent diagnostic performance of the MDS-MSA criteria, with improved diagnostic parameters compared to previous criteria and clinical diagnosis in practice. Clinically probable MDS-MSA was aimed to balance sensitivity and specificity and showed outstanding sensitivity (95.1%), specificity (94.0%), and diagnostic accuracy (94.3%). Clinically established MDS-MSA was aimed to achieve diagnostic certainty and showed perfect specificity even at early stages of the disease (100%). Despite the excellent diagnostic performance at final stages, sensitivity at early stages remains modest. Diagnosis in clinical practice only marginally improved compared to previous clinico-pathological studies, suggesting a need for reliable biomarkers to improve diagnostic accuracy. The excellent diagnostic properties of the MDS-MSA criteria did not change significantly when patients with parkinsonism or cerebellar ataxia were analysed separately. Our study's strength is the large cohort of patients with MSA, as well as the inclusion of non-MSA patients with other parkinsonian disorders and cerebellar syndromes with neuropathological confirmation of the diagnosis. Our data did not allow validation of the possible prodromal MDS-MSA criteria and studies to evaluate its diagnostic properties are warranted. In conclusion, the MDS-MSA diagnostic criteria outperformed previous diagnostic criteria and diagnosis by clinicians, and proved to be an accurate diagnostic tool in clinical practice and research.
Table 1. Proportion of patients meeting diagnostic criteria for multiple system atrophy according to different diagnostic criteria in 318 patients with parkinsonism or cerebellar syndrome with essential features for MSA at early (< 3 years of onset) and final stages of the disease.
Clinical parkinsonism(N = 248) |
Clinical cerebellar syndrome(N = 70) |
|||
Clinical diagnosis / diagnostic criteria |
Pathology confirmed-diagnosis |
|||
MSA* (%)(N = 55) |
Non-MSA** (%)(N = 193) |
MSA* (%)(N = 48) |
Non-MSA** (%)(N = 22) |
|
Early stage < 3 years |
||||
| MDS Clinically probable | 31 (56.4%) | 9 (4.7%) | 33 (68.8%) | 1 (4.5%) |
| MDS Clinically established | 7 (12.7%) | 0 | 14 (29.2%) | 0 |
| Second consensus - Possible | 31 (56.4%) | 21 (10.9%) | 31 (64.6%) | 4 (18.2%) |
| Second consensus - Probable | 23 (41.8%) | 4 (2.1%) | 18 (37.5) | 1 (4.5%) |
| Clinical diagnosis | 16 (29.1%) | 10 (5.2%) | 26 (54.2%) | 4 (18.2%) |
Final stage |
||||
| MDS Clinically probable | 52 (94.5%) | 11 (5.7%) | 46 (95.8%) | 2 (9.1%) |
| MDS Clinically established | 22 (40%) | 0 | 31 (64.4%) | 0 |
| Second consensus - Possible | 53 (96.5%) | 32 (16.6%) | 46 (95.8%) | 7 (31.8%) |
| Second consensus - Probable | 39 (70.9%) | 6 (3.1%) | 39 (81.3%) | 1 (4.5%) |
| Clinical diagnosis | 45 (81.8%) | 16 (8.3%) | 48 (100%) | 3 (13.6%) |
Legend: Results are presented by clinical presentation (parkinsonism and cerebellar syndrome) and pathological diagnosis (MSA vs non-MSA) in the columns. Proportion of patients meeting multiple system atrophy diagnostic criteria for each category are presented in those with pathological confirmation of the diagnosis of MSA (*true positives) and those with an alternative pathological diagnosis (**false positives).
Figure 1. Receiver operating characteristic (ROC) curves of each diagnostic category for multiple system atrophy at (A) early and (B) final stages.
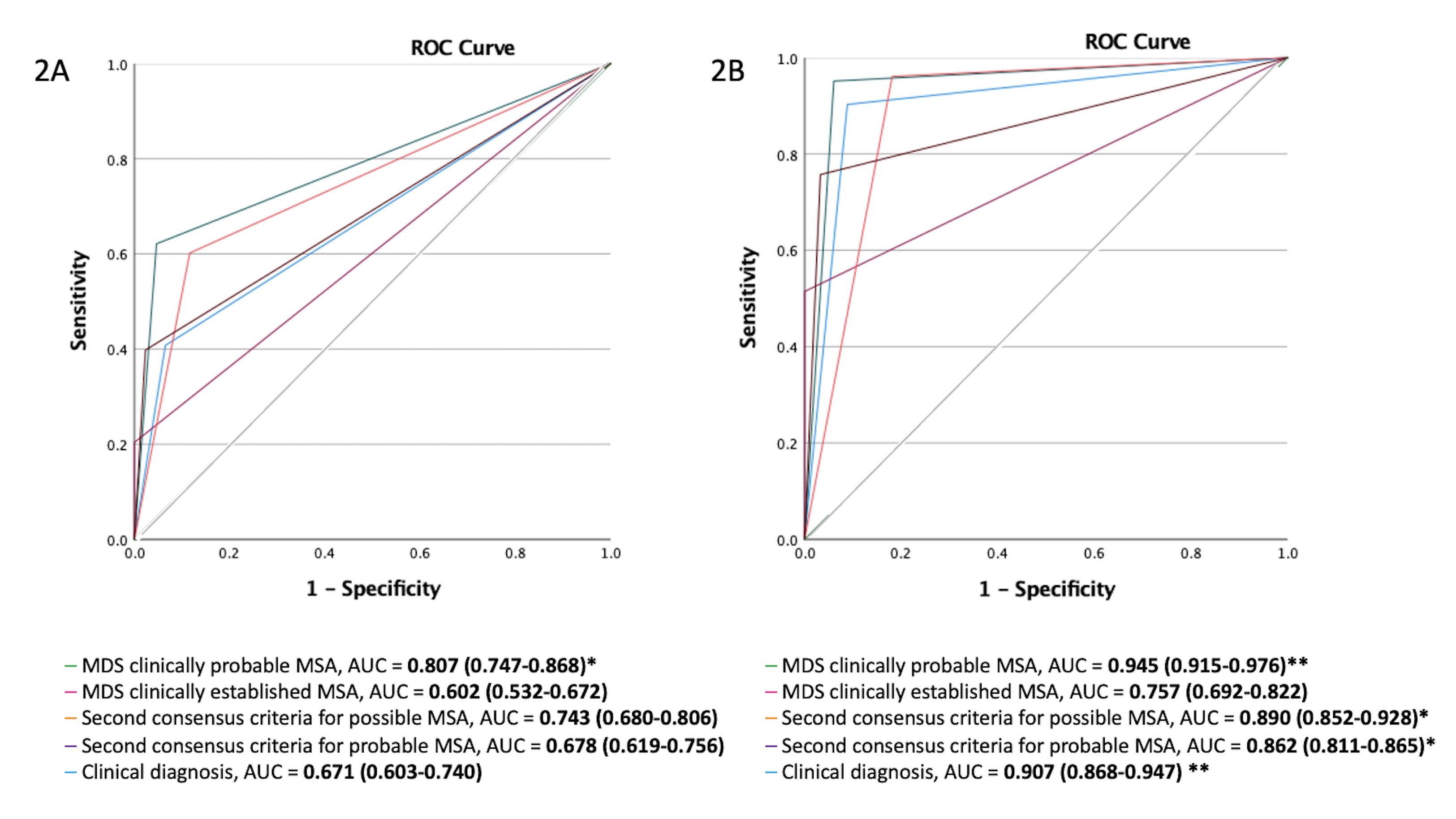
Legend: Clinically probable MDS-MSA showed the highest diagnostic accuracy at early stages, with a good area under the curve (AUC) score of 0.807. In contrast, second consensus possible MSA had a fair AUC score of 0.743, and second consensus probable MSA and clinical diagnosis had poor AUC scores of 0.687 and 0.671, respectively. At the final stage, clinically probable MDS-MSA and clinical diagnosis had excellent AUC scores of 0.945 and 0.907, respectively, with better overall diagnostic accuracy than second consensus possible and probable criteria, which both had good AUC scores of 0.890 and 0.862, respectively. Clinically established MDS-MSA had a poor AUC value of 0.602 at the early stage and a fair AUC value of 0.757 at the final stage, despite having excellent specificity due to its low sensitivity.
AUC, area under the ROC curve; ROC, receiver operating characteristic curve.
References
1. Virameteekul S, Revesz T, Jaunmuktane Z, Warner TT, De Pablo-Fernández E. Pathological Validation of the MDS Criteria for the Diagnosis of Multiple System Atrophy. Movement Disorders. 2023;38(3):444-452. doi:https://doi.org/10.1002/mds.29304
2. Osaki Y, Ben-Shlomo Y, Lees AJ, Wenning GK, Quinn NP. A validation exercise on the new consensus criteria for multiple system atrophy. Mov Disord. Nov 15 2009;24(15):2272-6. doi:10.1002/mds.22826
3. Koga S, Aoki N, Uitti RJ, et al. When DLB, PD, and PSP masquerade as MSA: an autopsy study of 134 patients. Neurology. Aug 4 2015;85(5):404-12. doi:10.1212/wnl.0000000000001807
4. Miki Y, Foti SC, Asi YT, et al. Improving diagnostic accuracy of multiple system atrophy: a clinicopathological study. Brain. Sep 1 2019;142(9):2813-2827. doi:10.1093/brain/awz189
5. Wenning GK, Stankovic I, Vignatelli L, et al. The Movement Disorder Society Criteria for the Diagnosis of Multiple System Atrophy. Mov Disord. Jun 2022;37(6):1131-1148. doi:10.1002/mds.29005
Read more Moving Along:






